In-Depth Exploration of Frozen Shoulder: Understanding Adhesive Capsulitis and Its Impact on Daily Life
Frozen shoulder, medically referred to as adhesive capsulitis, presents a complex and often excruciating challenge that can significantly disrupt daily routines and limit engagement in physical activities. This condition manifests through persistent pain and stiffness in the shoulder joint, making it difficult for individuals to carry out simple tasks or enjoy recreational activities. Typically, frozen shoulder develops gradually, often without any clear triggering event, and its symptoms can linger for months or even years, creating an ongoing cycle of discomfort. Early recognition and comprehensive understanding of this ailment are essential, as they enable timely medical interventions that can alleviate symptoms and improve the individual’s overall quality of life.
In our daily routines, we often overlook the critical role of shoulder mobility until faced with a condition like frozen shoulder, which sharply reminds us of its importance. The experience can evoke significant frustration and discomfort, akin to a loss of personal freedom in movement. Therefore, it is crucial to cultivate a deep understanding of frozen shoulder, as this knowledge not only highlights the extensive impact of the condition on our lives but also emphasizes the urgent need for effective treatment options focused on restoring functionality and relieving pain.
Phases of Frozen Shoulder: Comprehensive Strategies for Pain Relief and Recovery
The progression of frozen shoulder can be categorized into three essential phases: the freezing, frozen, and thawing phases. In the initial freezing phase, individuals typically experience a significant increase in pain alongside a gradual reduction in shoulder range of motion, making even simple daily tasks increasingly challenging. This decline in mobility can lead to profound feelings of helplessness and frustration as individuals struggle with activities that were previously second nature.
As the condition transitions into the frozen phase, while the pain intensity may stabilize, the limitations in mobility persist, further fueling ongoing frustration. The thawing phase marks a vital turning point in recovery, as individuals gradually begin to regain movement, albeit slowly over several months. By thoroughly understanding the different phases and their progression, we can underscore the importance of early diagnosis and proactive management strategies that can alleviate symptoms and facilitate recovery.
Essential Facts About Frozen Shoulder: Key Insights for Enhanced Awareness
- Frozen shoulder, clinically identified as adhesive capsulitis, is primarily marked by intense pain and stiffness in the shoulder joint, which severely affects mobility and daily activities.
- Common initiating factors for frozen shoulder include injury, overuse, and various underlying health issues such as diabetes and thyroid disorders.
- Individuals aged between 40 and 60 years, particularly women, are at an increased risk of developing frozen shoulder, often related to hormonal changes and other contributing factors.
- Typical symptoms include significant pain and stiffness, with diagnosis generally confirmed through thorough physical assessments and advanced imaging techniques.
- Treatment options for frozen shoulder range from conservative pain management and physical therapy to more invasive surgical interventions like manipulation under anesthesia or shoulder arthroscopy.
 Uncovering the Causes of Frozen Shoulder: Insights into Its Development
Uncovering the Causes of Frozen Shoulder: Insights into Its Development
The specific causes of frozen shoulder remain somewhat ambiguous; however, it is primarily associated with inflammation and thickening of the shoulder capsule, which is crucial for joint stability and movement. Factors such as injury or prolonged immobility—often following surgical procedures or due to other medical conditions—can trigger inflammation in this essential capsule.
This inflammatory response frequently leads to the formation of scar tissue, which can significantly hinder mobility and exacerbate pain. Although the underlying causes may differ from person to person, the resulting symptoms are generally debilitating and distressing. In addition to inflammation, various medical conditions—including diabetes, thyroid disorders, cardiovascular disease, and Parkinson's disease—have been linked to a higher risk of developing frozen shoulder. This highlights the importance of a comprehensive understanding of the condition's onset and effective management strategies.
Recognizing Key Risk Factors for Developing Frozen Shoulder
When exploring the risk factors associated with frozen shoulder, it becomes evident that certain demographics are more susceptible than others. Age is a significant determinant; individuals aged 40 to 60 years are notably more likely to encounter this condition. Furthermore, frozen shoulder is particularly prevalent among women, especially during menopause, when hormonal fluctuations can adversely affect the integrity of connective tissues.
Understanding these demographic patterns is crucial for identifying those who might benefit from proactive measures to protect shoulder health. A history of previous shoulder injuries or surgical procedures can also elevate the risk of developing frozen shoulder. Often, after surgery or trauma, individuals may unconsciously limit shoulder movement during recovery, increasing the likelihood of adhesive capsulitis.
Additionally, chronic health conditions, particularly diabetes and autoimmune disorders, can predispose individuals to frozen shoulder due to their effects on inflammation and the body's tissue repair processes. By recognizing these risk factors, individuals can take proactive steps to reduce the likelihood of experiencing this painful condition in the future.
 Understanding Symptoms and Diagnostic Procedures for Frozen Shoulder
Understanding Symptoms and Diagnostic Procedures for Frozen Shoulder
The symptoms associated with frozen shoulder can often be both perplexing and distressing for those affected. Initially, individuals may notice a dull ache in the shoulder that gradually intensifies over time. This discomfort can radiate down the arm, disrupting sleep and complicating even the most basic daily activities, such as reaching for items or dressing.
As the condition progresses, individuals may experience significant challenges with simple tasks, leading to increased frustration and a sense of helplessness. A defining characteristic of frozen shoulder is a pronounced limitation in the range of motion, which further complicates everyday life. Diagnosing frozen shoulder typically involves a thorough physical examination complemented by a detailed medical history.
Healthcare professionals will assess the range of motion and may perform specific tests to evaluate the extent of mobility limitations. Imaging studies, including X-rays or MRIs, may also be employed to eliminate other potential causes of shoulder pain. It is crucial for patients to maintain open communication with their healthcare providers about their symptoms and any prior injuries or conditions. A timely and accurate diagnosis is vital for initiating effective treatment strategies aimed at alleviating discomfort and restoring mobility.
Exploring Comprehensive Treatment Options for Effective Frozen Shoulder Management
When addressing frozen shoulder, a multifaceted approach is often essential for effectively managing pain and restoring mobility. Initially, conservative measures such as rest, ice application, and over-the-counter pain medications may be recommended to help control inflammation and alleviate discomfort. These early interventions can provide temporary relief while exploring additional rehabilitation options.
Early intervention is crucial; addressing symptoms promptly helps prevent further deterioration of the shoulder's range of motion. As treatment progresses, corticosteroid injections might be considered for more severe cases where pain management becomes increasingly challenging. These injections are particularly effective in reducing joint inflammation and providing significant temporary relief from pain.
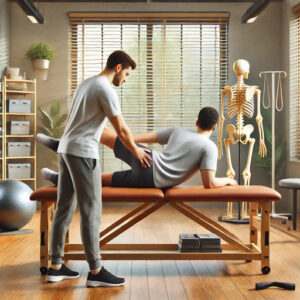
Moreover, physical therapy is frequently recommended as a fundamental aspect of the treatment strategy. Physical therapy focuses on personalized stretching and strengthening exercises tailored to individual needs, assisting in the restoration of mobility while minimizing discomfort. By incorporating various treatment modalities, individuals can aim for optimal outcomes in effectively managing frozen shoulder.
 The Critical Role of Physical Therapy and Exercises in Frozen Shoulder Rehabilitation
The Critical Role of Physical Therapy and Exercises in Frozen Shoulder Rehabilitation
Physical therapy is crucial in the recovery process from frozen shoulder, providing targeted interventions designed to enhance flexibility and strength in the affected shoulder joint. A qualified physical therapist will conduct a thorough assessment of individual needs and create a customized exercise program tailored to address specific limitations. Stretching exercises are particularly essential during this phase, as they work to elongate tight muscles and improve overall range of motion.
In addition to stretching, strengthening exercises that focus on surrounding muscles can provide better support for the shoulder joint. Beyond structured exercises, physical therapists may incorporate therapeutic modalities such as heat or ultrasound therapy to enhance blood circulation and promote healing within the joint. These techniques effectively alleviate pain while preparing muscles for movement.
As therapy progresses, maintaining consistency with a home exercise program is vital; dedication to rehabilitation is key to achieving lasting results. By actively engaging in our recovery journey, we empower ourselves to regain mobility and diminish the impact of frozen shoulder on our daily lives.
Evaluating Surgical Options for Frozen Shoulder: Important Factors to Consider
In certain cases where conservative treatments fail to provide sufficient relief or restore functionality, surgical intervention may become necessary. One commonly performed procedure for frozen shoulder is arthroscopic capsular release. During this minimally invasive surgery, the surgeon utilizes specialized instruments to cut the thickened capsule surrounding the shoulder joint, allowing for increased mobility and reduced pain.
While the prospect of surgery may seem daunting, it is generally reserved for situations where all other treatment avenues have been exhausted. Following surgical intervention, engaging in post-operative rehabilitation is crucial to ensure optimal recovery and regain strength and flexibility in the joint.
Our healthcare team will provide guidance throughout the entire process, assisting us in navigating any challenges that may emerge during recovery. Although surgical intervention may not be necessary for every individual with frozen shoulder, it represents a vital option for those who have not achieved relief through conservative therapies.
Implementing Effective Preventive Strategies for Frozen Shoulder: Essential Tips for Shoulder Health
Preventing frozen shoulder requires proactive measures to safeguard shoulder health throughout life. An effective prevention strategy includes maintaining an active lifestyle and integrating regular physical activities that promote shoulder flexibility and strength. Simple exercises, such as arm circles or gentle stretches, can help sustain joint mobility and avert stiffness.
Furthermore, individuals who have experienced an injury or undergone shoulder surgery must diligently adhere to prescribed rehabilitation exercises to ensure a complete recovery. Being aware of underlying health issues that could elevate the risk of developing frozen shoulder is equally important. For those managing diabetes or other chronic conditions, effectively controlling these health issues can significantly reduce the likelihood of complications associated with adhesive capsulitis.
By prioritizing overall health through regular check-ups and lifestyle modifications, we can take essential steps to prevent frozen shoulder from impacting our daily lives. Ultimately, awareness and proactive strategies are crucial components in protecting our shoulder health as we age.
If you're interested in discovering alternative treatment options for frozen shoulder, consider exploring cupping therapy. This alternative medical approach involves placing cups on the skin to create suction, which may alleviate pain and reduce inflammation. To learn more about how cupping therapy might benefit individuals with conditions like frozen shoulder, visit MCR Therapies' cupping therapy page. This resource provides comprehensive information about the procedure and its potential advantages.
Presented By: Expert Frozen Shoulder Therapy
The Article: Frozen Shoulder: Causes and Effective Treatment Options appeared first on https://mcrtherapies.co.uk
The Article Frozen Shoulder: Understanding Causes and Treatment Options appeared first on https://mcrtherapies.com
The Article Frozen Shoulder Causes and Treatment Options Explained Was Found On https://limitsofstrategy.com



Your exploration of frozen shoulder, or adhesive capsulitis, sheds light on a condition that many people may overlook until they experience its debilitating effects firsthand. The gradual nature of its onset is particularly perplexing, often leaving individuals confused and frustrated as they struggle to link their increasing discomfort to any specific event or activity. This experience resonates with me, as I witnessed a close friend go through a similarly harrowing journey. Initially diagnosed with a minor shoulder strain, months went by without significant improvement, leading to a deeper evaluation that ultimately revealed adhesive capsulitis.
Your exploration of frozen shoulder and its implications truly resonates with me. Having experienced shoulder issues myself, I can attest to how the gradual onset of pain and stiffness can sneak up on you, turning everyday activities into monumental tasks. It’s remarkable how something as seemingly simple as reaching for a glass can become a challenge, forcing one to reevaluate not just physical capabilities but one’s entire approach to daily life.
It’s great to hear your thoughts on this. The experience you described really highlights how our bodies can change without notice, turning the simplest tasks into significant hurdles. It’s a stark reminder that our physical well-being is intertwined with so much of our daily lives.
“I’m glad my article resonated with your experience—it’s truly eye-opening how much our shoulder mobility impacts daily life! If you’re interested, I found some helpful resources that could offer more insights and support on this journey.”
https://localseoresources.com/ninja
Your exploration of frozen shoulder really resonated with me. It’s striking how often we take our shoulder mobility for granted until faced with limitations. I remember a time when I injured my shoulder; simple tasks like reaching for a cup or even sleeping became challenging, and it made me rethink how much we rely on our bodies in daily life.