Comprehensive Guide to Understanding Plantar Fasciitis: Causes and Effective Treatment Approaches
Gain Insight into Plantar Fasciitis: An Overview of This Common Foot Condition
Plantar fasciitis is a widespread foot condition that affects millions globally, often resulting in severe pain and limiting everyday activities. This disorder typically targets active individuals aged between 25 and 65, manifesting as ongoing discomfort in the heel area. The condition arises when the plantar fascia, a thick band of connective tissue running across the bottom of the foot, experiences overstretching or strain. High levels of physical activity or prolonged standing can diminish the fascia's elasticity and resilience, leading to inflammation and sharp pain, particularly around the heel. Understanding plantar fasciitis is essential for those seeking effective relief and treatment strategies, as it can significantly improve their ability to engage in daily tasks without discomfort or pain.
Key Diagnostic Tests for Accurately Identifying Plantar Fasciitis
How to Obtain a Thorough Diagnosis for Plantar Fasciitis
Achieving an accurate diagnosis of plantar fasciitis necessitates a comprehensive physical examination by a qualified healthcare professional. During this in-depth evaluation, the clinician will discuss your specific symptoms and conduct a meticulous examination of your feet to identify visible signs of distress. They may gently press on your plantar fascia to assess inflammation and gauge your pain response. Open communication about your daily discomfort is vital, particularly regarding when and where the pain is most pronounced. In many cases, plantar fasciitis can be diagnosed based solely on clinical evaluation. However, if your doctor suspects other underlying issues, they might suggest imaging studies, like X-rays, to eliminate other potential causes of your foot pain.

Recognizing the Key Symptoms Associated with Plantar Fasciitis
The symptoms of plantar fasciitis can emerge gradually or appear suddenly, particularly after engaging in rigorous physical activities. Early detection of these symptoms is crucial for prompt intervention and effective treatment. The severity and duration of symptoms can vary significantly among individuals. The most prevalent symptom is localized pain in the sole of the foot near the heel, which can range from a dull ache to a sharp, stabbing sensation. Additionally, discomfort may be felt in the arch of the foot, often described as a burning feeling. Many individuals report acute pain upon waking or after prolonged periods of inactivity, typically accompanied by stiffness that resolves after a few minutes of movement. Other common symptoms include increased pain following physical exertion, tenderness when pressure is applied to the affected area, and noticeable foot stiffness, particularly after sleep or sitting for extended durations.
Diving Into the Root Causes of Plantar Fasciitis
Plantar fasciitis develops when the plantar fascia, the robust band of tissue on the foot's underside, undergoes overstretching or excessive strain due to repetitive activities like prolonged standing or running. This condition may also arise from sudden weight gain, often observed during pregnancy. The continuous stress on the plantar fascia can cause chronic degeneration or micro-tears in the fascial fibers, particularly at the insertion point on the calcaneus or heel bone. These micro-tears can lead to inflammation and pain that can greatly hinder mobility and daily life. Diagnostic imaging techniques, such as ultrasonography, can demonstrate thickening and calcification of the plantar fascia, indicating more severe manifestations of this painful condition.
Identifying Risk Factors That Increase the Likelihood of Developing Plantar Fasciitis
- Foot arch abnormalities (including both flat feet and high arches)
- Long-distance runners or individuals frequently jogging on downhill or uneven terrain.
- Being overweight or experiencing rapid weight gain.
- A tight or overstretched Achilles tendon.
- Wearing shoes that lack adequate arch support or have overly soft soles.
- Sudden changes in physical activity levels or intensity.
Critical Steps for Accurately Diagnosing Plantar Fasciitis
If you suspect you are experiencing plantar fasciitis or are dealing with persistent foot pain, it is essential to consult your healthcare provider for a comprehensive diagnosis and personalized treatment plan. Early intervention can dramatically enhance your comfort and overall quality of life. Your doctor will thoroughly examine your foot, looking for specific symptoms or risk factors associated with plantar fasciitis. They will evaluate areas of heightened tenderness beneath the heel bone, assess your foot arch type, and check for limited dorsiflexion, which refers to the upward movement of the ankle.
In addition to a thorough physical examination of your foot, your healthcare provider may recommend X-rays or ultrasound imaging if they suspect other injuries or conditions, such as heel spurs or arthritis. These imaging techniques can help visualize the plantar fascia, revealing signs of thickening or inflammation, which are common indicators of this condition. If conservative treatments do not provide relief, your doctor may suggest advanced imaging techniques like magnetic resonance imaging (MRI) to rule out other potential issues.
Examining a Variety of Effective Treatment Options for Plantar Fasciitis
Many individuals suffering from plantar fasciitis can expect to see improvement within nine to twelve months after initiating non-surgical treatment approaches. Recognizing that the effectiveness of these treatments can vary based on the individual’s specific condition and adherence to the prescribed regimen is crucial.
Common Non-Surgical Treatment Strategies to Consider:
Rest. The first and most essential step in managing plantar fasciitis is to refrain from activities that exacerbate the pain. Allowing the plantar fascia to heal is critical during this recovery period. Instead, consider engaging in low-impact activities like cycling or swimming, which place significantly less stress on your feet compared to walking or running.
Ice. Applying ice to the affected area is a highly effective way to reduce inflammation and alleviate pain. Utilizing a cold water bottle or ice pack on the painful area for 15 to 20 minutes three times a day, especially after activities that worsen your pain, can provide significant relief.
Stretching. Tightness in the foot and calf muscles can aggravate plantar fasciitis symptoms. Incorporating targeted stretching exercises into your daily routine can help lengthen these muscles, thereby reducing strain on the plantar fascia and promoting overall flexibility.
Night splints. Wearing night splints can gently stretch the plantar fascia while you sleep, preventing the tissue from tightening overnight and reducing morning stiffness and pain. Although it might take some time to get used to wearing a splint, many individuals report substantial relief from heel pain as a result.
Footwear choices. Choosing supportive shoes that offer adequate cushioning and arch support is vital for managing plantar fasciitis pain. Avoid footwear lacking proper support or that are excessively worn. If discomfort persists, consult your doctor about custom orthotics, which can provide additional support tailored to your foot's specific needs.
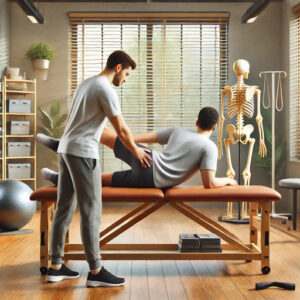
Physical therapy. Your healthcare provider may recommend a structured exercise program with a physiotherapist focused on stretching the calf muscles and implementing specific plantar fascia therapy. Additionally, physical therapy may involve cold treatments, massage, and other therapeutic modalities aimed at alleviating inflammation in the plantar fascia.
Nonsteroidal anti-inflammatory medications (NSAIDs). Over-the-counter NSAIDs, such as ibuprofen, can help relieve pain and inflammation. However, it is essential to use these medications under the guidance of a healthcare professional and for a limited duration to prevent potential side effects.
If Conservative Treatments Fail, Your Doctor May Propose:
A walking boot and crutches. These assistive devices may be prescribed temporarily to allow adequate rest and healing for your foot.
Corticosteroid injections. For severe pain and inflammation that do not respond to conservative treatments, corticosteroid injections may be utilized. While these injections can offer temporary relief, they are usually administered cautiously due to the risk of weakening the plantar fascia and potential complications.
Extracorporeal shockwave therapy (ESWT) is another non-invasive treatment option that delivers high-energy shock waves aimed at promoting healing in the plantar fascia. However, this treatment may not be suitable for everyone, and its effectiveness can vary.
Botulinum toxin injections involve using a protein derived from the bacteria Clostridium botulinum. These injections can help relax the tissue surrounding the plantar fascia, thereby alleviating pain and discomfort.
Dry needling employs a sterilized needle to stimulate myofascial trigger points in the affected area. While the effectiveness of dry needling for plantar fasciitis remains debated, some studies suggest it may help reduce pain severity and improve overall function.
Low-level laser therapy. This option may be considered by your healthcare provider to alleviate pain and inflammation associated with plantar fasciitis. Research indicates that this therapy can provide relief from heel pain for several months, enhancing overall mobility.
Foot surgery is typically regarded as a last resort for individuals who do not respond to non-surgical treatment options. Although surgical intervention can provide relief, it carries inherent risks and the potential for chronic pain, making it a decision that necessitates careful consideration.

Selecting the Ideal Footwear for Effective Management of Plantar Fasciitis
Choosing the right footwear is crucial for effectively managing plantar fasciitis. Wearing appropriate shoes can greatly reduce the risk of developing or worsening this painful condition, thereby promoting overall foot health.
When searching for shoes beneficial for plantar fasciitis, consider the following essential characteristics:
Arch support. Sufficient arch support helps distribute weight evenly across the foot, alleviating pressure on the plantar fascia and minimizing discomfort during various physical activities.
Cushioning. Shoes that offer ample cushioning in the arch and forefoot areas assist in shock absorption and lessen strain on the plantar fascia, ensuring each step is more comfortable and reducing the likelihood of further injury.
Heel support. Look for shoes with a sturdy heel counter, as the heel sustains significant impact upon landing, which can contribute to microtrauma in the fascia. Soft silicone heel cushions can provide additional support and comfort.
Shock absorption. Opt for footwear with excellent shock-absorbing properties, particularly in the heel area. Cushioned soles or gel insoles can enhance shock absorption, further protecting the plantar fascia from damage and strain.
Consulting with a podiatrist or orthopedic specialist for personalized recommendations tailored to your unique foot structure and the severity of your plantar fasciitis is advisable. Additionally, consider custom-made or over-the-counter orthotic inserts, which can help evenly distribute pressure across your feet, effectively reducing pain and discomfort.
Incorporating Effective Stretching Exercises to Relieve Plantar Fasciitis Symptoms
Research indicates that specific stretching exercises targeting plantar fasciitis can significantly assist in pain relief as part of a comprehensive treatment strategy. Notably, studies have shown that participants who engaged in regular stretching routines over eight weeks experienced a remarkable 52% reduction in heel discomfort. Maintaining flexibility in the calf muscles is vital for preventing the onset of plantar fasciitis, as tightness can exacerbate symptoms.
To maximize your stretching routine, aim to perform these exercises three times daily: in the morning, before lunch, and before bedtime.
Calf stretch. Stand facing a wall, keeping one leg straight behind you with the heel flat on the ground. Bend the other knee and lean forward, pushing your hips toward the wall. You should feel a stretch in the calf of the straight leg. Hold this position for 15 to 30 seconds, then switch legs to ensure balanced flexibility.
Plantar fascia stretch. While seated, place one foot flat on the floor. Lift your other leg and position your ankle across your knee in a figure-four posture. Grasp the toes of the elevated foot and gently pull them back towards you, feeling a stretch in the sole of your foot. Use your other hand to gently massage the stretched area. Hold for 10 seconds and repeat this stretch ten times on each foot to maintain flexibility and reduce pain.
It is essential to remember that while these exercises can be beneficial, they should not substitute professional medical advice from your healthcare provider or other qualified practitioners. Always consult your doctor for personalized guidance and treatment options tailored to your specific needs.
The post Plantar Fasciitis – Identifying Effective Treatments appeared first on MCR Therapies.
The Article Plantar Fasciitis: Discovering Effective Treatment Options appeared first on https://mcrtherapies.com
The Article Plantar Fasciitis Treatment: Explore Effective Solutions Was Found On https://limitsofstrategy.com



This guide on plantar fasciitis certainly highlights a condition that’s all too familiar for many of us, especially those who lead active lifestyles. Personally, I found myself struggling with this issue last year after ramping up my running routine. The persistent heel pain not only affected my ability to exercise but also impacted my mental well-being, as I felt sidelined from activities I enjoyed.
This is such an important topic! I recently dealt with plantar fasciitis myself, and it really opened my eyes to how much we take our feet for granted. I found that incorporating specific stretching routines and strengthening exercises made a significant difference in my recovery. It’s fascinating how something that seems so localized can affect our entire lifestyle and well-being.
I really appreciate the comprehensive approach you’ve taken to discussing plantar fasciitis. It’s a topic that seems to be gaining attention as more people recognize how common this condition is, and for good reason—its impact on daily life can be quite profound. I’ve personally experienced the discomfort it can cause, especially when my routine involves long hours on my feet, whether it’s at work or during recreational activities like hiking or running.
It’s interesting to hear how personal experiences with plantar fasciitis can really shape our understanding of it. That discomfort can definitely disrupt daily life, especially for those of us who find ourselves on our feet for extended periods—it’s like a constant reminder to take care of our bodies.
It’s interesting how plantar fasciitis is becoming more well-understood as awareness grows. It’s one of those conditions that can sneak up on you, especially for those of us with active lifestyles. I can relate to the discomfort you’ve described—long hours on your feet can really take a toll. I’ve found that wearing more supportive footwear during those extended periods makes a difference, but then there’s a balance to strike with style and function.
It’s great to hear that the article resonated with you. Plantar fasciitis can indeed disrupt daily activities in ways that are often underestimated. When you’re on your feet for long hours, whether working or enjoying outdoor pursuits, it can feel like an unwelcome shadow following you around.
I really appreciate this comprehensive look at plantar fasciitis. I’ve dealt with it myself for a few years now, and it’s interesting to hear that it primarily affects active individuals. I never thought of myself as particularly hardcore in terms of physicality, but I guess those long hours at my standing desk and the occasional weekend hike really did a number on my feet!
It’s interesting to consider how plantar fasciitis not only affects individual mobility but also influences overall quality of life. I encountered this firsthand when a close friend, an avid runner, developed the condition and had to change their training routine dramatically. It highlighted the importance of preventative measures, like proper footwear and stretching techniques, even for those who are active.